Speaker Profile
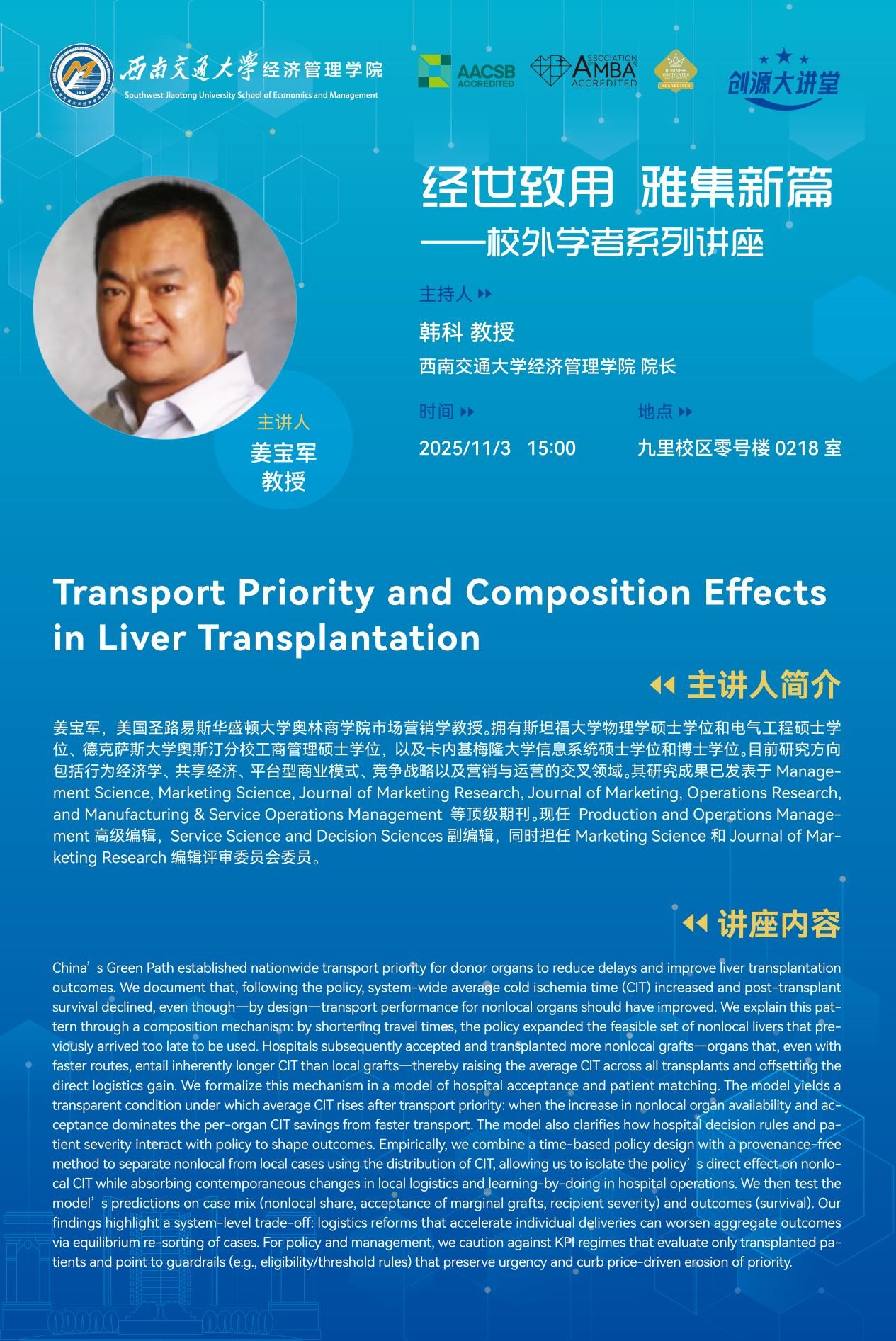
Dr. JIANG Baojun is a Professor of Marketing at the Olin Business School, Washington University in St. Louis. He holds Master's degrees in Physics and Electrical Engineering from Stanford University, an MBA from University of Texas at Austin, and both an M.S. and a Ph.D. in Information Systems from Carnegie Mellon University.
His research interests include behavioral economics, the sharing economy, platform-based business models, competitive strategy, and the interface of marketing and operations. His work has been published in premier journals such as Management Science, Marketing Science, Journal of Marketing Research, Journal of Marketing, Operations Research, and Manufacturing & Service Operations Management.
Currently, Professor Jiang serves as a Senior Editor for Production and Operations Management, an Associate Editor for Service Science and Decision Sciences, and is on the editorial review boards of Marketing Science and Journal of Marketing Research.
Abstract
China’s Green Path established nationwide transport priority for donor organs to reduce delays and improve liver transplantation outcomes. We document that, following the policy, system-wide average cold ischemia time (CIT) increased and post-transplant survival declined, even though—by design—transport performance for nonlocal grafts should have improved. We explain this pattern through a composition mechanism: by shortening travel times, the policy expanded the feasible set of nonlocal livers that previously arrived too late to be used. Hospitals subsequently accepted and transplanted more nonlocal grafts—organs that, even with faster routes, entail inherently longer CIT than local grafts—thereby raising the average CIT across all transplants and offsetting the direct logistics gain. We formalize this mechanism in a model of hospital acceptance and patient matching. The model yields a transparent condition under which average CIT rises after transport priority: when the increase in nonlocal organ availability and acceptance dominates the per-organ CIT savings from faster transport. The model also clarifies how hospital decision rules and patient severity interact with policy to shape outcomes. Empirically, we combine a time-based policy design with a provenance-free method to separate nonlocal from local cases using the distribution of CIT, allowing us to isolate the policy’s direct effect on nonlocal CIT while absorbing contemporaneous changes in local logistics and learning-by-doing in hospital operations. We then test the model’s predictions on case mix (nonlocal share, acceptance of marginal grafts, recipient severity) and outcomes (survival). Our findings highlight a system-level trade-off: logistics reforms that accelerate individual deliveries can worsen aggregate outcomes via equilibrium re-sorting of cases. For policy and management, we caution against KPIs that evaluate only transplanted patients and point to guardrails (e.g., eligibility/threshold rules) that preserve urgency and curb price-driven erosion of priority.
Date/Time: November 3, 2025, 15:00 p.m.
Venue: Room 0218, 0 Teaching Building, Jiuliu Campus